By JACOB REIDER
I haven’t blogged this but, which kinda surprises me, since I discover myself describing it typically.
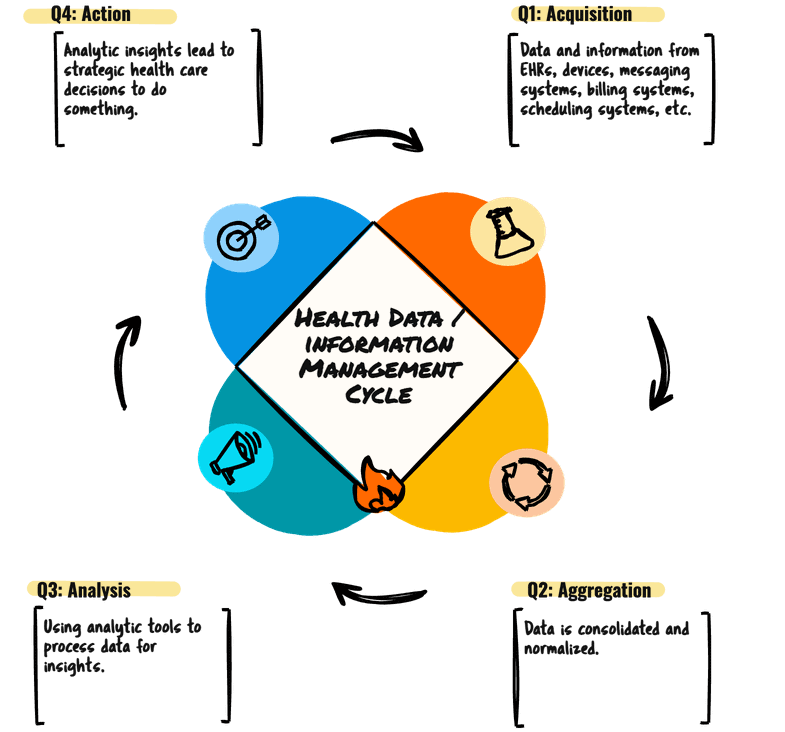
Let’s begin with an outline. We are able to take a look at well being data by means of the lens of a lifecycle.
The promise of Well being Info Know-how has been to assist us – ideally to attain optimum well being within the folks we serve.
The idea @ the start of the HITECH act was: “ADOPT, CONNECT, IMPROVE.”
These had been the three pillars of the Significant Use Incentive applications.
Undertake expertise so we will join techniques and subsequently enhance well being.
Easy, sure?
Years later, one can argue that adoption and even connection have (largely) been completed.
However the bridge between measurement and well being enchancment isn’t one we will simply cross with the present instruments obtainable to us.
Why?
Lots of the technical options, significantly people who promote dashboards, are lacking essentially the most essential piece of the puzzle. They get us shut, however then they drop the ball.
And that’s the place this “easy”AAAA” mannequin turns into helpful.
For information and data to be actually priceless in well being care, it wants to finish a full cycle.
It’s not sufficient to simply gather and show. There are 4 important steps:
1. Purchase. That is the place we collect the uncooked information & data. EHR entries, machine readings, patient-reported outcomes … the gamut of data flowing into our techniques. Notice that I differentiate between information (transduced representations of the bodily world: blood stress, CBC, the DICOM illustration of an MRI, drugs really taken) and data (diagnoses, concepts, signs, the issue record, drugs prescribed) as a result of information is reliably true and data is presumably true, and presumably inaccurate. We have to weigh these two sorts of inputs correctly – as information is a significantly better enter than data. (I’ll resist the temptation to go off on a vector about information being a preferable enter for AI fashions too … maybe that’s one other put up.)
2. Mixture. As soon as acquired, this information and data must be introduced collectively, normalized, and cleaned up. That is about making disparate information sources converse the identical language, making a unified repository so we will ask questions of 1 dataset reasonably than tens or a whole bunch.
3. Analyze. Now we will begin to make sense of it. That is the place medical determination help (CDS) begins to take form, how we will determine traits, flag anomalies, predict dangers, and spotlight alternatives for intervention. The analytics part is the place most present options finish. A dashboard, an alert, a report … all of them dump recommendation – like a bowl of spaghetti – into the lap of a human to kind all of it out and work out what to do.
Positive … you may see patterns, perceive populations, and determine areas for enchancment … All good issues. The maturity of well being data expertise signifies that aggregation, normalization, and complicated evaluation are actually much more accessible and strong than ever earlier than. We not want a dozen specialised level options to deal with every step; fashionable platforms can combine all of it. That is good – however not adequate
A dashboard or analytics report, irrespective of how elegant, is finally passive. It reveals you the reality, nevertheless it doesn’t do something about it.
Act. That is the place the rubber meets the street. It’s about translating insights into tangible interventions. What ought to occur (or not occur) subsequent?
What good is understanding a affected person is at excessive danger for readmission if that information doesn’t set off a particular follow-up protocol, a social work session, or an adjusted discharge plan? What’s the purpose of figuring out a prescribing sample if the system doesn’t facilitate a change in observe, present fast suggestions to clinicians, or regulate order units?
We now have relied on human intervention to bridge this hole. A clinician may see a pattern on a report after which manually provoke a change. We see a necessity for screening and make an order … (one-by-one-by-one).
So unhappy.
The true energy of well being IT, particularly with the developments we’ve seen, lies in closing this loop. We must be constructing techniques that not solely purchase, mixture, and analyze information but additionally facilitate the following finest motion, prioritizing what’s finest for the particular person we serve, and (in fact) who must be the recipient of this steering?
Think about a system that not solely flags a possible difficulty but additionally:
* Routinely generates a personalised affected person training doc.
* Suggests an up to date remedy order (or a set of orders) with one click on.
* Schedules a follow-up appointments with the suitable specialists .
* Pushes a notification to a care coordinator to intervene.
This isn’t about eradicating human judgment; it’s about empowering it. It’s about making the correct factor to do the simplest factor to do.
The fantastic thing about this cycle is its iterative nature.
The actions we take then generate new information and data, feeding again into the “Purchase” part, permitting us to repeatedly refine our understanding and enhance our interventions. And the quicker and extra continuously we will cycle by means of these 4 steps, the extra responsive, environment friendly, and patient-centric our well being care groups turn out to be.
Subsequent time you’re evaluating a brand new Well being IT resolution, ask the essential query: how does this method assist us Act?
Jacob Reider MD is a household doctor who beforehand served as Deputy Nationwide Coordinator at ASTP/ONC, CMIO at Allscripts and Albany Medical Middle, CEO of Alliance for Higher Well being and at the moment doing angel investing, advising and pickleballing. Discover his occasional ideas at http://www.docnotes.net which is among the few blogs older than THCB!